Protein Digestion
Protein digestion occurs in the stomach and the small intestine. Reaction arrows are in red. The enzymes involved are in italics and label the relevant reaction arrows. The activation of enzymes are indicated by black arrows.
Protein Digestion in the Stomach
Pepsinogen, the inactive form of pepsin, is secreted (solid-headed dashed arrow) by chief cells (labeled circle) that line the gastric glands. This enzyme is activated (black reaction arrow) by hydrogen ions, H+. These ions are from the hydrochloric acid secreted (solid-headed dashed arrow) by parietal cells that also line the gastric glands.
Proteins are long chains of amino acids. The enzyme pepsin hydrolyzes proteins into fragments of various sizes called peptides; some amino acids are also produced in this manner. This indicated by the red reaction arrow.
Protein Digestion in the Small Intestine
Hydrolysis of peptides from the stomach continues by the action of three 'proteases' secreted (solid-headed arrows) in pancreatic juice. These 'proteases' are inactive until they reach the lumen of the small intestine; they are procarboxypeptidase, chymotrypsinogen, and trypsinogen. Their activations are indicated by theblack reaction arrows.
The enzyme enterokinase is membrane-bound along the lining of this region of the small intestine. It convertstrypsinogen into its active form trypsin. Trypsin catalyzes the conversion of both procarboxypeptidase andchymotrypsinogen into their active forms, carboxypeptidase and chymotrypsin, respectively. These are represented by the black reaction arrows with 'trypsin' written atop them.
The enzyme chymotrypsin, like pepsin, hydrolyzes peptides in various size smaller amino acid chains finally producingdipeptides & tripeptides. Carboxypeptidase specifically hydrolyzes the amino acid from the carboxyl end of peptide chains to yield individual amino acids. These reactions are indicated by red reaction arrows.
Amino acids are transported through the cells lining the small intestine and into the blood. The small peptides are transported into the cells lining the small intestine where intracellular peptidases (labeled outside symbolic GI tract) convert them into amino acids that then enter the blood.


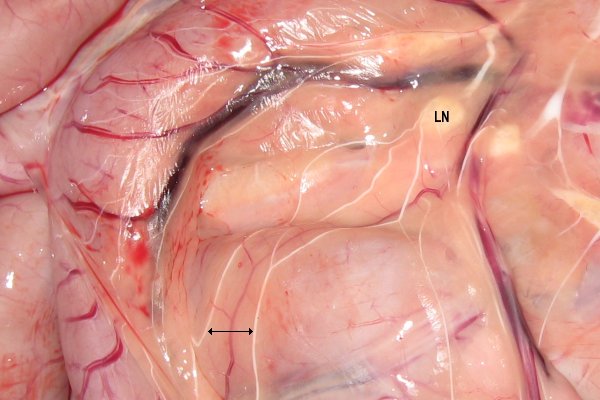 Another lipid of importance that is absorbed in the small intestine is cholesterol. Cholesterol homeostatis results from a balance of cholestrol synthesis, absorption of dietary cholesterol, and
Another lipid of importance that is absorbed in the small intestine is cholesterol. Cholesterol homeostatis results from a balance of cholestrol synthesis, absorption of dietary cholesterol, and